Diabetes can increase your risk of developing certain eye conditions. One of these conditions is diabetic retinopathy, affecting over 4 million Americans.
Diabetic retinopathy is generally not reversible, but its progression can be slowed or stopped with proper management and treatment.
Managing diabetic retinopathy can include:
- Controlling blood sugar
- Blood pressure and cholesterol management
- Booking regular eye exams
Treatment options for diabetic retinopathy can include:
- Medication
- Laser eye surgery
- Vitrectomy
Talk to your optometrist and help protect your vision.
How Can Diabetes Affect Your Ocular Health?
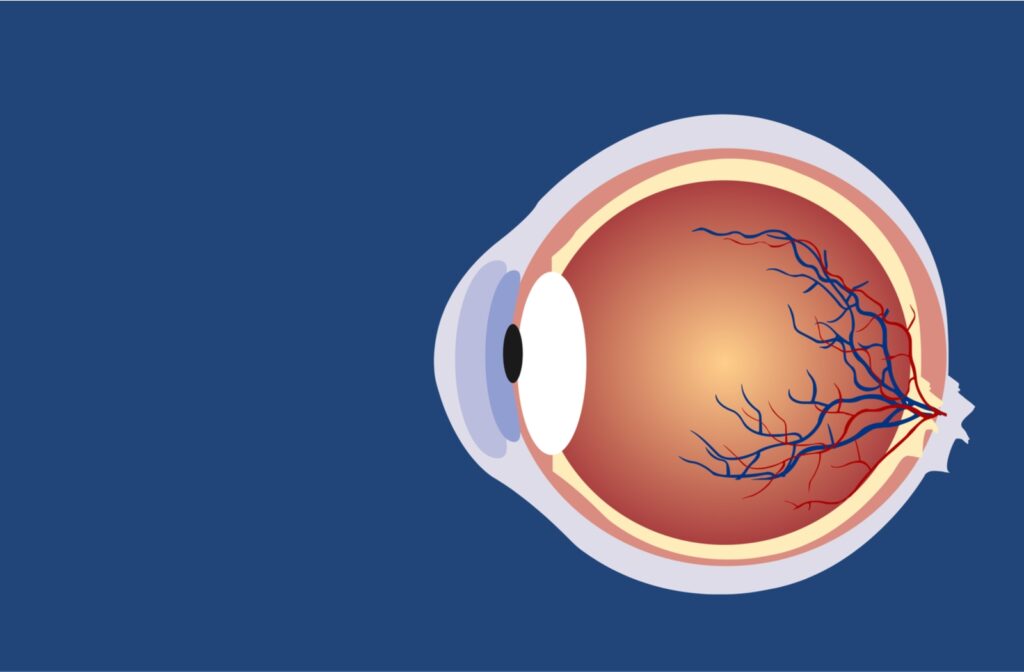
Your eyes are supported by various blood vessels in your retina. These blood vessels are sensitive to high blood sugar, putting them at risk of damage if you have diabetes.
Blood vessels may swell, break, and leak fluid if your blood glucose levels are high for long periods. Damaged blood vessels can lead to severe vision loss.
What Is Diabetic Retinopathy?
Diabetic retinopathy is a complication of diabetes where damage occurs to the blood vessels within your retina. This part of your eye is essential for helping you see, and complications affecting the retina may result in blindness.
Someone can develop diabetic retinopathy if they have type 1 or type 2 diabetes. It’s the most common cause of vision loss for people with diabetes. This condition typically affects both of your eyes.
Diabetic retinopathy can scar and damage your retina if not treated. Unfortunately, the early stages of this condition may not present any noticeable symptoms. In later stages, you may experience:
- Central vision loss
- Inability to see colors
- Blurry vision
- Holes or black spots in your vision
- Floaters in your visual field
Stages of Diabetic Retinopathy
There are 2 main types of this condition: nonproliferative and proliferative diabetic retinopathy. Nonproliferative diabetic retinopathy is the initial stage of this condition, worsening with time:
- Nonproliferative diabetic retinopathy: This stage occurs when microaneurysms protrude from the walls of the blood vessels in your eyes—these bulges can break & lead fluid into the retina
- Proliferative diabetic retinopathy: When this condition progresses, damaged blood vessels can close off, promoting abnormal, weaker blood vessel development
As damage to the blood vessels in the retina continues, this condition may progress to diabetic macular edema.
Diabetic Macular Edema
Diabetic macular edema is a complication of diabetic retinopathy caused by consistently high blood sugar. Leaking fluid can cause swelling in the macula. This swelling occurs because of fluid buildup.
What Causes Diabetic Retinopathy?
Diabetic retinopathy develops when your blood sugar levels are too high, leading to a blockage in the blood vessels in your retina, cutting off its blood supply. Your body then attempts to grow new blood vessels. However, these blood vessels develop abnormally and break, leaking fluid and blood.
Who Is At-Risk of Diabetic Retinopathy?
Anybody with diabetes can develop diabetic retinopathy, but some people are more at risk. You’re more likely to develop this condition if you:
- Have uncontrolled blood sugar levels
- Have high blood pressure
- Have high cholesterol
- Are pregnant
- Regularly smoke
- Have had diabetes for a long time
Diabetic retinopathy can severely damage your vision, leading to potential vision loss. If you have diabetic retinopathy, is this condition reversible?
Is Diabetic Retinopathy Reversable?
Damage caused by diabetic retinopathy is typically permanent. This condition isn’t fully reversible, but some treatments may help bring some of your vision back. While treatments aren’t likely to return your vision, your eye doctor can help prevent your vision from worsening.
Diabetic Retinopathy Treatment
The right treatment for your condition depends on several factors. When creating your customized treatment plan, your optometrist will take your age, medical history, visual acuity, and retinal damage into consideration.
Some ways to address diabetic retinopathy include:
Medical Control
Learning to control your blood sugar and blood pressure can help prevent future vision loss. You should carefully maintain the diet provided to you by your doctor and take your diabetes medication. It’s possible that controlling your blood sugar may help recover some of your vision.
Medicine
Medication can help reduce swelling, slow vision loss, and potentially improve your vision. A common medication for diabetic retinopathy is known as anti-VEGF medication, such as:
You receive anti-VEGF medication through injections in the eye. Another possible treatment is steroid injections. Your eye doctor can determine the most effective medication for your needs and how many injections you require.
Laser Surgery
Laser surgery can help seal off blood vessels leaking fluid, reducing retinal swelling. These blood vessels then shrink and cannot grow further.
Vitrectomy
In the later stages of diabetic retinopathy, your optometrist may recommend vitrectomy. During this treatment, your doctor surgically removes the vitreous gel, scar tissue, and blood from your eye that prevents light from focusing properly.
No matter the type of treatment your eye doctor recommends, they can help you address diabetic retinopathy and preserve your vision.
Protect Your Vision for the Future
If you have diabetes, have an annual examination at minimum. Even if you can see fine, conditions like diabetic retinopathy can develop with limited symptoms. An early diagnosis can prevent severe vision loss. Visit your eye doctor if you have symptoms of diabetic retinopathy or require an eye exam. Book an appointment today.